The influence of the cornea on visual acuity results - Important indicators in eyeglass prescription
3/12/20257 min read
Understanding Visual Acuity and Its Importance
Visual acuity refers to the clarity or sharpness of vision and is a fundamental aspect of visual perception. Typically measured in terms of a fraction, such as 20/20 vision, visual acuity encompasses the ability to recognize shapes, details, and letters at a specified distance. This measurement is critical not only in assessing general vision health but also in guiding eyeglass prescriptions for individuals who require corrective lenses.
The importance of visual acuity extends into various facets of daily life. Good visual acuity enables individuals to perform routine activities such as reading, driving, and engaging in professional tasks. In educational settings, strong visual clarity can significantly impact a student's learning experience and performance. As such, maintaining optimal visual acuity is essential for achieving overall effectiveness in daily engagements.
To evaluate visual acuity, several standard tests are employed, including the Snellen chart, which is the most commonly used method. During this test, individuals read letters of varying sizes from a designated distance, helping to quantify their visual sharpness. Additionally, other assessments, such as the LogMAR chart and the ETDRS chart, offer further refinements in measuring visual acuity, particularly for research and clinical purposes. These tests allow eye care professionals to determine the exact strength of prescription lenses needed to correct any deficiencies in vision.
Overall, understanding visual acuity is crucial for both eye health professionals and individuals seeking to improve their sight. By recognizing the importance of clear vision, one can appreciate how meticulously measured visual acuity impacts the determination of eyeglass prescriptions, ultimately leading to better visual outcomes in daily life.
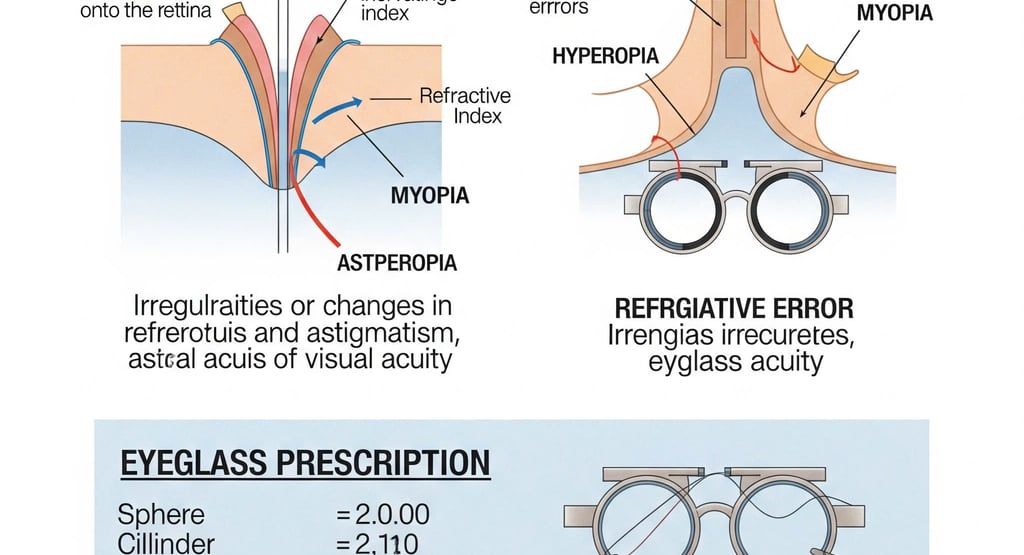
The Anatomy of the Eye: Focus on the Cornea
The cornea is the outermost layer of the eye, playing a critical role in the overall visual system. Comprising five distinct layers—the epithelium, Bowman's layer, stroma, Descemet’s membrane, and the endothelium—the cornea serves as both a protective barrier and a crucial refractive surface. By curving outward, it facilitates the bending of incoming light rays, thereby assisting in their accurate focusing on the retina. This curvature is essential for achieving optimal visual acuity, as even slight irregularities can lead to distorted images or blurred vision.
One of the primary functions of the cornea is to provide a significant amount of the eye's total optical power, which is approximately 43 diopters. The refractive index of the cornea is vital for ensuring that light enters the eye at the appropriate angle. A well-shaped cornea results in precise refraction, enabling clear eyesight. However, various factors may influence the corneal curvature, including genetics and environmental influences, potentially leading to conditions such as astigmatism or keratoconus.
In addition to its refractive duties, the cornea is also responsible for protecting the internal structures of the eye. It is avascular, meaning it does not contain blood vessels, relying instead on the tear film and aqueous humor for nourishment. This characteristic aids in maintaining transparency, which is essential for proper vision. However, diseases such as corneal dystrophies, infections, or injuries can compromise the cornea, affecting its ability to refract light adequately, and thus impairing visual acuity. Understanding the intricate anatomy and function of the cornea is fundamental in the field of optometry, as it directly impacts eyeglass prescriptions and overall visual health.
How Corneal Shape Affects Visual Acuity
The shape and thickness of the cornea play a crucial role in determining visual acuity, influencing how light is refracted as it enters the eye. The cornea is a transparent layer that covers the front of the eye and contributes significantly to overall optical power, accounting for approximately two-thirds of the eye's total focusing ability. Variations in corneal shape can lead to refractive errors such as astigmatism, which can severely impact visual clarity.
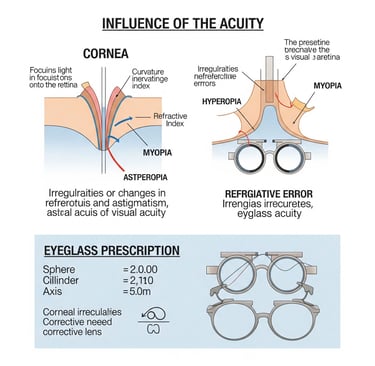
Corneal astigmatism arises when the curvature of the cornea is uneven, resulting in distorted or blurred vision. In such cases, light rays entering the eye are focused at multiple points rather than a single point on the retina, necessitating corrective lenses. Eye care professionals assess corneal shape during comprehensive eye exams using a number of diagnostic tools, such as corneal topography, which maps the surface curvature. This evaluation allows eye specialists to determine the extent of astigmatism and the appropriate adjustments needed in eyeglass prescriptions.
Another significant condition related to corneal shape is keratoconus, a progressive thinning of the cornea that leads to a conical shape. This abnormality can cause significant visual distortions and further complicates the prescription process. Individuals with keratoconus may require specialized contact lenses or other surgical options in addition to traditional eyeglasses. Thus, a thorough evaluation of corneal characteristics is vital in tailoring prescriptions to meet the individual needs of patients.
Understanding the relationship between corneal shape and visual acuity is imperative, as it directly influences how light is perceived and ultimately affects the effectiveness of prescribed eyewear. Consequently, eye care providers must remain vigilant in evaluating corneal characteristics to ensure that their patients receive the most accurate visual correction possible.
Corneal Refraction and Its Role in Eyeglass Prescription
The cornea is a transparent, dome-shaped surface that covers the front of the eye and plays an essential role in refracting light. When light enters the eye, it first passes through the cornea, which is responsible for approximately 70% of the eye's total optical power. The corneal curvature and its refractive index significantly influence how light is bent, allowing it to focus on the retina for clear vision. Any irregularities in this process can lead to refractive errors, which may impact visual acuity and necessitate the use of corrective lenses.
Corneal refractive errors such as myopia (nearsightedness), hyperopia (farsightedness), and astigmatism occur when the light entering the eye does not focus correctly on the retina. For instance, in myopia, the cornea may be too steep, causing distant objects to appear blurry. Conversely, in hyperopia, the cornea could be too flat, blurring close objects. Astigmatism arises when the cornea has an irregular shape, leading to distorted vision at all distances. Identifying these refractive errors is crucial in determining the appropriate eyeglass prescription.
The measurement of corneal topography has become a vital component in eyeglass prescription calculations. Advanced technology, including corneal mapping, allows eye care practitioners to assess the curvature and surface variations of the cornea comprehensively. These measurements are critical to formulating an accurate eyeglass prescription, enabling practitioners to address any aberrations that affect visual acuity. By meticulously assessing corneal refraction, eye care professionals can optimize vision correction for individuals, ensuring that their eyeglasses provide the clearest and most comfortable vision possible.
Diagnostic Tools for Assessing Corneal Influence
In the realm of ocular health, accurately assessing the cornea's condition is paramount, particularly when determining its influence on visual acuity. Eye care professionals employ an array of diagnostic tools that provide invaluable insights into corneal morphology and functionality. Among these, corneal topographers stand out as essential instruments. These devices create detailed maps of the cornea's surface, capturing variations in curvature and elevation. Such cartographic representation enables eye care specialists to detect irregularities, including corneal astigmatism, which can significantly impact one's visual quality.
Corneal topography not only aids in the diagnosis of refractive errors but also assists in pre-surgical evaluations for procedures such as LASIK or keratoplasty. The precise data gathered from these assessments guide practitioners in crafting tailored treatment plans, aligning with the patient's unique corneal characteristics.
Complementing topographic assessments, pachymeters play a critical role in evaluating corneal thickness. This measurement is crucial as it can influence intraocular pressure readings and overall corneal health. A pachymeter accurately measures the central corneal thickness (CCT), allowing clinicians to determine the risk of diseases such as glaucoma and to make informed decisions regarding surgical interventions. Variations in corneal thickness are essential indicators that can point to underlying pathologies, impacting a patient’s visual acuity.
Moreover, integrating these diagnostic tools provides a comprehensive understanding of how corneal properties affect vision. As advancements in technology continue to evolve, eye care professionals gain enhanced capabilities to analyze corneal characteristics thoroughly. Therefore, the use of corneal topography and pachymetry not only fosters expert insight into visual acuity assessments but also contributes significantly to the broader field of ophthalmology, ensuring that patients receive the most accurate prescriptions for their unique needs.
Implications for Eyeglass Prescription: Case Studies
The relationship between corneal health and visual acuity is foundational in optometry, influencing the lens prescription for eyeglasses. Examining real-world case studies can provide valuable insights into how varying corneal conditions affect individual prescriptions. This discussion will highlight different patient scenarios to illustrate these implications.
Consider the case of a 45-year-old female patient diagnosed with keratoconus, a condition characterized by the progressive thinning and bulging of the cornea, leading to distorted vision. Upon examination, her corneal topography displayed significant irregularities. Traditional spherical lenses were deemed insufficient, prompting the optometrist to prescribe specialized toric lenses that catered to the specific corneal shape, effectively enhancing her visual acuity.
In another scenario, a 60-year-old male patient presented with pellucid marginal degeneration, another corneal disorder that affects the clarity of vision. His examination revealed a marginal thinning of the cornea, which complicated standard eyeglass prescriptions. After careful assessment, the practitioner recommended customized rigid gas-permeable lenses that complemented the optical irregularities, resulting in vastly improved visual performance.
A distinct case involved a young woman experiencing myopia largely due to astigmatic changes in her cornea. The optometrist's approach included a comprehensive evaluation of both visual acuity and corneal curvature. The resultant eyeglass prescription incorporated a combination of corrective lenses that addressed her astigmatism while optimizing her overall vision. By precisely aligning the prescription with her corneal structure, her daily visual tasks witnessed significant enhancement.
These examples underline the vital role of corneal assessments in developing accurate eyeglass prescriptions. By considering unique corneal conditions, eyecare professionals can tailor their approach, ensuring patients receive appropriate lens solutions to improve their visual acuity and overall quality of life.
Future Trends in Corneal Research and Eyewear Solutions
As we move further into the 21st century, there is a growing interest in the exploration of corneal research and its implications for visual acuity and eyewear solutions. Enhanced understanding of the cornea's structure and function is leading to innovative approaches in eyecare. Researchers are increasingly focusing on the biochemical properties of the cornea, utilizing advanced imaging techniques and biomaterials to explore how these factors influence visual outcomes.
One significant trend in corneal research is the development of new technologies for surgical interventions. Procedures such as corneal cross-linking are gaining popularity, offering a method to strengthen weakened corneal tissue and improve refractive stability. Moreover, advancements in laser technology are allowing for more precise reshaping of the cornea, which can enhance visual acuity beyond traditional methods. These innovations not only aim to treat existing conditions like keratoconus but also provide preventive measures for individuals at risk of corneal degeneration.
In addition to surgical approaches, the market for contact lenses is evolving rapidly. New materials and designs, including scleral lenses and ortho-k treatments, are being introduced to address specific corneal irregularities and restore clear vision without the need for glasses. These contact lenses offer improved fit and comfort, along with customizations tailored to individual corneal profiles, allowing for a more focused correction of refractive errors.
Furthermore, ongoing research into the role of the cornea in overall ocular health is shedding light on the relationship between systemic diseases and corneal conditions. This knowledge is driving the development of integrated care strategies that consider both corneal integrity and systemic health for more effective management of visual acuity issues.
Collectively, these trends signal a promising future for corneal research and eyewear solutions. As science continues to unravel the complexities of the cornea, the potential for improved visual outcomes and the enhancement of life quality through innovative eyecare solutions becomes increasingly viable.
