Is refraction without eye drops accurate? - Evaluating the eyeball axis - the factor that determines myopia
3/13/20257 min read
Understanding Refraction and Its Importance in Eye Care
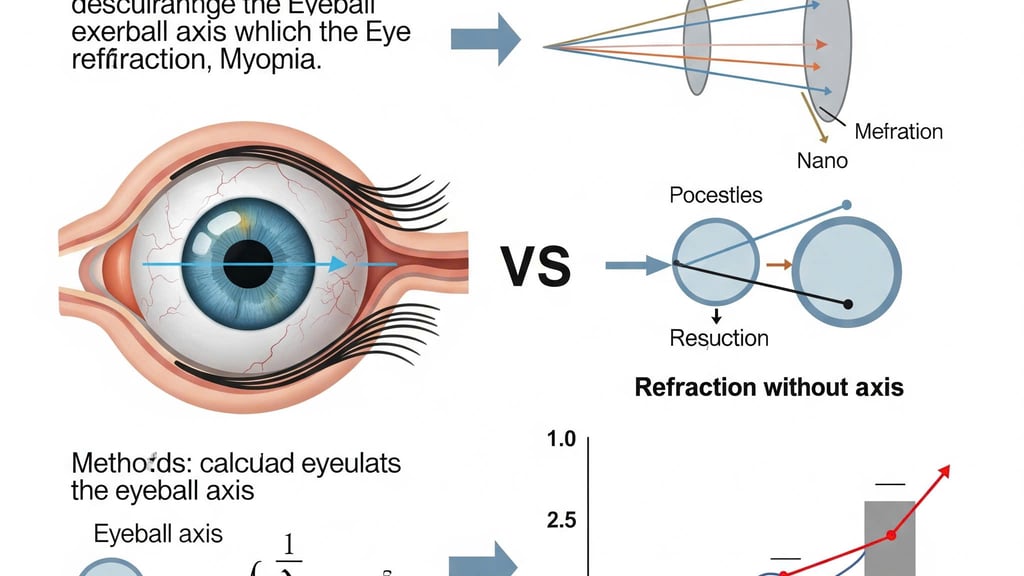
Refraction is a crucial process in eye care that involves measuring how light rays bend as they pass through the eye. This bending, or refraction, is essential for focusing images clearly on the retina, thus allowing us to see well. When light enters the eye, it is refracted through the cornea and the lens. Refraction tests are typically conducted during an eye examination to evaluate a person's vision and determine any visual impairments such as myopia, hyperopia, or astigmatism.
The standard method of performing refraction includes the use of various tools, particularly a phoropter, which allows the optometrist to change the lens strength and find the optimal prescription for corrective lenses. During refraction, the individual is instructed to focus on an eye chart while the practitioner assesses their ability to discern letters at various distances. This procedure can be performed with or without the use of eye drops, which help to temporarily dilate the pupils and improve the clarity of vision, particularly in cases of latent refractive errors.
Refraction is significant not only for prescribing corrective lenses but also for diagnosing various refractive errors. Myopia, or nearsightedness, is one of the most common conditions assessed through refraction. It occurs when the eyeball is longer than normal, causing distant objects to appear blurry. Accurate refraction is vital for determining the degree of myopia and creating an appropriate prescription. This process aids in understanding the individual's vision needs, ensuring that proper corrective measures are utilized for maintaining optimal eye health.
Understanding Myopia and Its Measurement
Myopia, commonly known as nearsightedness, is a refractive error that results in distant objects appearing blurred while close objects can be seen clearly. This condition occurs when the eyeball is longer than normal or the cornea has excessive curvature, leading to light rays focusing in front of the retina instead of directly on it. Symptoms may include difficulty seeing road signs, squinting, and eye strain, particularly during activities that require long-distance vision.
The causes of myopia are multifaceted, involving genetic predisposition as well as environmental factors. Studies indicate a significant hereditary component, with children of myopic parents having a higher likelihood of developing the condition. Additionally, prolonged near work activities, such as reading and using electronic devices, have been implicated in the rising prevalence of myopia in recent decades, particularly in urban populations. Data shows that myopia affects approximately 30% of adults in the United States, and rates are even higher in certain Asian countries, indicating a global public health concern.
Measuring myopia accurately is crucial for effective management and treatment. The primary method involves assessing visual acuity using a standardized eye chart. Furthermore, refraction tests are conducted using objective techniques, such as autorefractors, or subjective methods, involving the patient’s feedback with a phoropter. Central to these measurements is the eyeball axis, which refers to the length and shape of the eye. Variations in the eyeball axis significantly influence refractive outcomes and can impact the accuracy of measurements. For instance, a longer axial length is typically associated with higher degrees of myopia.
In conclusion, understanding myopia—including its symptoms, causes, and methods of measurement—is essential for addressing this widespread visual impairment. As the prevalence continues to rise, particularly among young populations, the need for effective strategies for early detection and intervention becomes increasingly important.
The Role of Eye Drops in Refraction Tests
Eye drops play a crucial role in the process of refraction testing, particularly when cycloplegic agents are employed. These agents are designed to temporarily paralyze the ciliary muscle, which is responsible for the eye's ability to focus. By inhibiting the ciliary muscle, eye drops facilitate a more accurate measurement of refractive error, allowing eye care professionals to assess the true refractive state of the eye without the interference of accommodation, the eye’s natural focusing mechanism. This is especially important in cases where the refractive error is not immediately apparent, such as in young patients or those with high levels of myopia.
The use of cycloplegic eye drops is typically indicated in a variety of scenarios. For instance, they are commonly employed in comprehensive eye examinations for children, as accommodating responses may mask underlying refractive errors. Additionally, these drops can assist in cases where patients exhibit significant variability in their refractive measurements, helping to ensure a consistent and reliable result. It is worth noting that when these drops are applied, patients may experience temporary blurred vision and sensitivity to light, effects that usually subside within a few hours. Therefore, practitioners often advise patients to arrange transportation following the examination.
Despite the advantages offered by cycloplegic drops, there are potential drawbacks to consider. Some patients may experience adverse reactions, such as allergic responses or discomfort. Additionally, the temporary nature of the ciliary muscle paralysis may lead to a reluctance in some patients to undergo the procedure, particularly those who are anxious about the effects of eye drops. Nonetheless, the benefits of achieving an accurate refraction measurement through the use of eye drops generally outweigh these concerns, highlighting their indispensable role in the evaluation of myopia and other refractive errors.
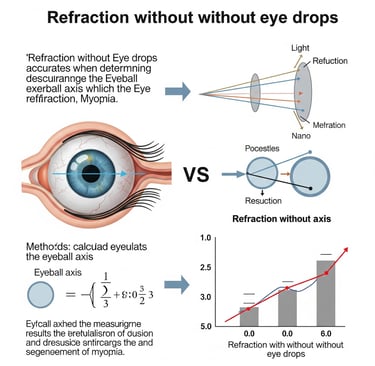
Evaluating Refraction Accuracy Without Eye Drops
The accuracy of refraction conducted without the application of eye drops has been an ongoing topic of debate among optometrists and ophthalmologists, particularly for patients with myopia. Traditional refraction methods often employ cycloplegic agents to temporarily paralyze the ciliary muscle, allowing for a more precise measurement of the eye’s refractive error. This practice is particularly vital for individuals with myopia, as their ability to accommodate can significantly alter the results obtained through standard refraction techniques. Without such pharmaceutical intervention, the accuracy of the measurements may be jeopardized.
Several studies have sought to elucidate the reliability of non-cycloplegic refraction. Research indicates that while some practitioners are able to obtain acceptable refraction results without eye drops, particularly in adults, discrepancies remain significant in pediatric populations. A study published in a leading optometry journal highlighted that children demonstrate a marked variability in their refractive outcomes when cycloplegic agents are not utilized. Consequently, this could lead to a misdiagnosis of myopia levels, resulting in either overcorrection or undercorrection when prescribing corrective lenses.
Expert opinion also plays a pivotal role in this discussion. Many specialists advocate for the use of eye drops in cases where accurate refraction is crucial, particularly for young patients or those with fluctuating vision. While some argue that skilled practitioners might achieve reliable results through careful techniques without drops, the consensus leans toward the understanding that cycloplegia provides a necessary safeguard to ensure more consistent and trustworthy measurements. Thus, the overall accuracy of non-cycloplegic refraction remains contentious, and practitioners are encouraged to consider the specific needs and conditions of individual patients while weighing the benefits and drawbacks of using eye drops in the refraction process.
Eyeball Axis: What It Is and Why It Matters
The eyeball axis is a crucial anatomical feature of the human eye, referring to the line that extends from the anterior to the posterior segment. In simpler terms, it is the measure of the eye's length, typically assessed from the cornea to the retina. This distance is vital as it plays a significant role in the overall refractive status of the eye. The eyeball axis may vary among individuals, and these variations can directly influence refractive errors, particularly myopia (nearsightedness).
Understanding the eyeball axis is essential for eye care professionals when evaluating the structure and function of the eye. Anatomically, the eye is composed of various elements, including the cornea, lens, and retina, all working together to focus light correctly onto the retina. If the eyeball's axis is too long, light rays focus in front of the retina, leading to myopia. Conversely, if the axis is too short, hyperopia (farsightedness) may occur. Thus, recognizing the parameters of the eyeball axis is vital in diagnosing and managing these conditions effectively.
Research has shown that as the length of the eyeball increases, the likelihood of developing myopia also rises, particularly in children and adolescents. This relationship highlights the importance of conducting accurate measurements of the eyeball axis during comprehensive eye exams. Moreover, variations in the axis can lead to differing refractive outcomes and may affect the reliability of refraction methodologies, especially without the use of cycloplegic eye drops. Understanding how the eyeball axis interacts with other ocular structures is crucial to tailoring appropriate myopia management strategies and enhancing patient care.
Factors Influencing Myopia Development
Myopia, commonly known as nearsightedness, is a refractive error that has been the subject of extensive research. Aside from the physical measurements of the eyeball axis, several other factors influence the development and progression of this condition. Genetics play a vital role, as familial patterns of myopia are frequently observed in clinical studies. Individuals with parents who are myopic have an increased likelihood of developing the condition themselves. Studies indicate that specific genetic markers may be associated with refractive errors, highlighting the complexity of heredity in myopia.
Environmental influences are equally significant and merit thorough examination. Prolonged near-work activities, like reading, use of computers, or playing video games, are prevalent in modern lifestyles. These activities require the eyes to focus at close range for extended periods, potentially contributing to myopia development. Conversely, a lack of exposure to natural light has also been implicated. Studies have shown that spending time outdoors reduces the risk of developing myopia and may even halt its progression. This prompts inquiries into how urban living and lifestyle choices can contribute to refractive errors.
Lifestyle choices further extend the discussion on myopia's development. Factors such as excessive screen time, inadequate outdoor activity, and poor visual ergonomics during tasks can exacerbate the condition. Interventions aimed at improving eye health, such as regular eye exercises, proper lighting during tasks, and scheduled breaks during prolonged near-work, are essential for mitigating risks. Understanding these various influences provides a multifaceted perspective on myopia, emphasizing that it is not solely determined by the anatomy of the eye, but rather a complex interplay of genetic, environmental, and lifestyle factors that shape one’s refractive outcomes.
Conclusion: Weighing the Accuracy of Refraction Techniques
The evaluation of refraction techniques, particularly those performed without the use of eye drops, reveals a multifaceted approach to understanding myopia. Throughout this discussion, we have explored various factors influencing the accuracy of refraction, focusing significantly on the eyeball axis. The complexity of ocular anatomy, combined with individual variations in refractive error, necessitates a careful examination of the conditions under which refraction is performed. It becomes evident that while refraction without eye drops can yield valuable insights, it may not always result in the most accurate prescription for corrective lenses.
Research indicates that certain patients, particularly those with established myopia, might exhibit variations in their refractive measurements when not administered cycloplegic agents. This highlights the importance of considering factors such as age, degree of myopia, and even environmental influences that can affect the accuracy of both subjective and objective refraction. Eye care practitioners should recognize these nuances and adapt their refraction strategies accordingly, potentially employing a hybrid approach that considers both non-cycloplegic and cycloplegic methods.
Furthermore, there is a need for ongoing research in this domain. Future studies should aim to quantify the impact of not using eye drops during refraction, particularly in populations with high myopia prevalence. By establishing protocols that standardize these practices, eye care professionals can enhance the accuracy of refraction outcomes. As the field of optometry evolves, integrating evidence-based practices with technological advancements will be critical in refining our understanding of refractive techniques and optimizing patient care. Addressing the questions surrounding the accuracy of refraction without eye drops will ultimately contribute to better vision correction strategies for individuals with myopia.
